Optical biopsy shines light on prostate cancer
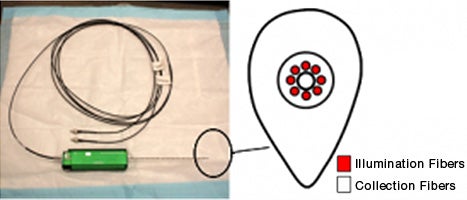
How many angels can dance on the head of a pin? If the pin is a biopsy needle in the lab of Priya Werahera, Ph.D., the answer is nine: eight fiber-optic strands to deliver light into the prostate and one central fiber to read the tissue’s fluorescence.
“It’s a step forward in the way we diagnose prostate cancer,” said Werahera, investigator at the University of Colorado Cancer Center and assistant professor in the departments of pathology and bioengineering at the University of Colorado. “What we did is redesign the inner needle of a standard prostate biopsy needle and insert a fiber-optic probe at its tip.”
A bit like a police officer’s radar gun, this fiber-optic probe emits light and reads the reflection. Because tumor tissue fluoresces differently than healthy tissue, the fiber-optic eye can see if and where cancer resides inside the prostate — in real time prior to extracting a tissue sample. The technology is moving toward market in collaboration between Colorado startup Precision Biopsy and Boston biotech Allied Minds. Precision Biopsy recently secured $2.5 million in funding to kick off the commercialization phase.
In the early 1990s, Werahera’s first project at the CU Cancer Center was to develop 3-D computer models of the prostate, i.e., digital replicas of prostates based on nine or 10 cross-sectional slices per specimen. These digital prostates and images of likely cancers within helped treatment teams decide on the need for further diagnostics, including mapping biopsies, in which a grid of prostate samples are taken in search of a cancer’s exact position.
Indirectly, Werahera’s current project brings the idea full circle — using the optical biopsy needle, Werahera can map the prostate as a grid, but has the added ability to only pull tissue samples from the grid holes that optically test positive for cancer. It’s like looking for plastic submarines in the game Battleship. With the single core sample of a traditional biopsy, it’s easy to miss one of these tiny, two-peg submarines; by optically scanning holes placed every five millimeters, Werahera’s grid has the ability to detect 95 percent of prostate cancers.
Precision biopsy technology might also have applications in treatment.
“Currently, surgeons don’t know the margins of prostate tumors they operate on,” Werahera said. “So they keep cutting until they excise all the cancerous tissue with a margin of healthy tissue.”
This work is assisted by a pathologist in the operating room who examines excised tissue for signs of cancer. When the excised tissue tests healthy, the surgeon stops cutting. Werahera’s optical biopsy needle might soon enable surgeons to determine tumor margins in real-time during surgeries, helping them cut only until the optical signs of cancer disappear. In follow-up care, the optical needle can help probe for recurrence.
In full, the device — developed by Werahera in collaboration with mechanical engineer John Daly, pathologists Scott Lucia and Francisco La Rosa, clinical urologists David Crawford and Fernando Kim, and more than 20 members of the University of Colorado Prostate Cancer Research Laboratory — consists of the re-engineered biopsy needle with a fiber-optic probe, the standard biopsy gun and a small electronic device that reads tissue fluorescence from the needle’s fiber-optic probe to tell the doctor whether cancer exists in the surrounding tissue.
“Engineering can make a substantial difference in how physicians manage this disease,” Werahera said. “With Precision Biopsy technology, we use engineering and mathematics to identify prostate cancer in real-time. How to use that information is up to the doctor.”